One in ten people in the US currently has diabetes and the incidence is growing such that the CDC projects that as many as one in three people in the US may have diabetes in 2050! As such, the prevalence of Diabetic eye disease is likely to increase. Diabetes can impact the eye by increasing the risk of cataract, glaucoma, and diabetic retinopathy. However, good blood sugar control and annual dilated eye exams by an eye physician can detect and treat these findings early to prevent loss of vision.
What is Diabetic Retinopathy?
Diabetic retinopathy results from sustained uncontrolled blood sugars over several years which damage blood vessels nourishing the retina. The retina is the light sensitive film lining the back of the eye that translates light into images. Diabetic vascular damage in the retina may result in swelling, bleeding, and scar tissue formation within the retina.
Development of Diabetic Retinopathy
Persistent suboptimal blood sugar control can weaken the blood vessels nourishing the retina resulting in bleeding and leakage of fluid into the retina. If the leakage impacts the central part of the retina known as the macula, diabetic macula swelling (edema) ensues and central vision may become blurred and distorted. As the retinopathy progresses, the damage to the retinal blood vessels may ultimately result in closure and poor perfusion to the peripheral retina. This may result in the development of abnormal new frail blood vessels that may tear and bleed into the eye clouding the vision and leading to scar tissue formation. This scar tissue can pull on the retina and lead to retinal detachment with loss of vision.
Who’s at risk of Diabetic Retinopathy?
All patients with diabetes (type 1, type 2, and gestational) are at risk of diabetic retinopathy. Risk of retinopathy onset and progression increases with poorly controlled blood sugars, duration of diabetes (most patients will develop some form of retinopathy by 15 years), associated uncontrolled high blood pressure & cholesterol, active smokers, and diabetic patients going through puberty/pregnancy.
How to prevent Diabetic Retinopathy?
While diabetic retinopathy isn’t always preventable, following up for regularly scheduled exams is one of the most important ways to prevent vision loss. Most diabetic patients should expect to develop some form of diabetic retinopathy in their lifetime if they live long enough. Currently, only about 60% of people with diabetes have yearly screenings for diabetic retinopathy. Patients with Type 1 diabetes should have annual screenings for diabetic retinopathy beginning 5 years after the onset of their disease, whereas those with Type 2 diabetes should have a prompt examination at the time of diagnosis and at least yearly examinations thereafter. Maintaining a healthy diet with controlled blood sugars, blood pressure, & cholesterol in the range advised by your doctor are also important factors. Avoidance of cigarette smoking and regular exercise help to keep the blood vessels healthy.
What are the symptoms of Diabetic Retinopathy?
Most forms of early diabetic retinopathy are without symptoms. The disease often progresses unnoticed until it affects vision. As a result, you may be unaware your eyes are harmed until the problem is very advance. Symptoms of diabetic retinopathy may include floaters, blurred & distorted central vision, cloudy vision, and loss of parts or all of your vision. Fortunately, your doctor can detect and treat problems early if you schedule regular eye exams before diabetic retinopathy leads to irreversible vision loss. “An ounce of prevention is worth a pound of cure.
How to treat Diabetic Retinopathy?
Once diabetic retinopathy is detected, your doctor may obtain ancillary tests to guide in the management of your condition. If early stage retinopathy is detected, your doctor may suggest observation with more frequent follow up exams to monitor for progression. Stricter maintanence of blood sugar control may be advised. Should your retinopathy require definitive therapy, your doctor may advise photocoagulation laser, medicated injections, and/or surgery.
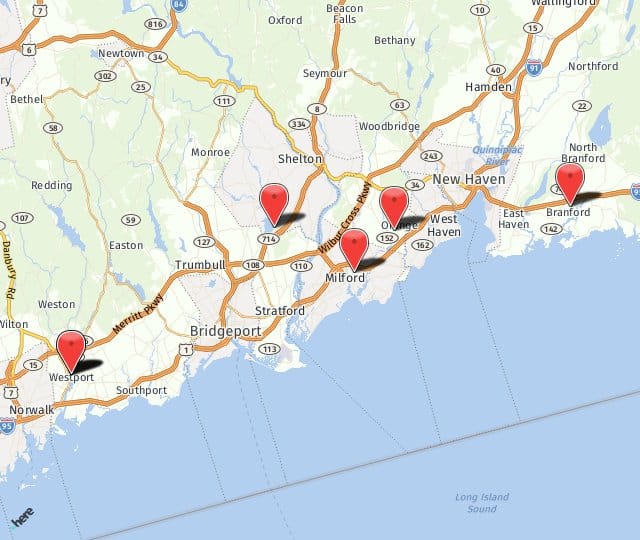
Blog posted by Dr. David Levinson a board certified ophthalmologist and fellowship trained medical and surgical retina specialist. For more information on floaters, flashes, retinal detachment, or any of the services we offer, please contact us (203) 878-1236 at any of our 4 offices in Milford, Orange, Branford, or Shelton. We’re looking forward to hearing from you soon.